Brain on Fire: The Role of Toxic Mold in Triggering Psychiatric Symptoms
March 14, 2014
By Mary Ackerley, M.D.
Editor’s Note: Dr. Mary Ackerley is an integrative psychiatrist who recently obtained certification in the Shoemaker Protocol used to treat toxic mold illness. She did her M.D. at the University of Maryland; her medical residency at Johns Hopkins; her M.D.H. at the American Medical College of Homeopathy; and her undergraduate degree at Harvard University. She practices in Tucson. The following is a slightly shortened transcript of a recent talk she gave to a group of physicians and researchers interested in the health effects of toxic mold.
I get asked all the time, “How did a psychiatrist get interested in mold?”
My interest really stems from my clinical experience. As an integrative psychiatrist, I attract people who are not able to be helped easily by traditional meds. They go to their doctors, they’re given some Zoloft or Prozac or Xanax. Not only does it not do anything, often times it makes them worse. So they start to seek out someone like me, who’s willing to work with different methods.
Although people complain of depression and anxiety, I often find that fatigue and muscle and joint pain are the stronger complaints. Those are complaints that are usually ignored by traditional busy family practitioners because it’s all lumped together under the heading of “Depression.”
I was doing a CME credit on depression, and the case study was a woman with joint and muscle pain, fatigue, back muscle pain, anxiety and depression. The whole thing was that you were supposed to learn to diagnose all these somatic complaints as depression.
But in fact, what I do is the opposite.
Eventually I began to realize that I was attracting some patients who told me they were mold patients. They came to me with strange labs and even stranger protocols. I was pretty traditional in just looking at it and saying, “I don’t know what this stuff means.” Then I would start to work on their depression and anxiety.
For me, quite frankly, I grew up on Long Island on the east coast, and I really thought that mold was natural and not a big deal. Every basement smelled moldy.
But I was kind of curious, and I eventually got one of Dr. Shoemaker’s books because patients were handing them to me.
First Experience Treating Mold
Then one day, a patient that I’d known pretty well for a couple of years arrived really late for her appointment. She was a woman in her seventies and she was usually pretty well put together. Now she was pretty disheveled and confused. She told me she couldn’t even remember how to get to the office, which was very strange. She’d had the same problem with another physician and drove around the block for an hour, and couldn’t remember how to get to the office.
I was actually pretty concerned. She’d been seeing me for mild depression and a tremor. We’d been doing some supplements that had been helping, but the tremor hadn’t been touched.
She told me that over the past few weeks, she’d seen a few other doctors. She had referred herself to an ENT because her sinusitis was acting up. She had referred herself to a dermatologist because now she had this strange rash on her shins which concerned her. She also was having problems with some aches and pains.
I was definitely concerned, so concerned that I made a note that I was going to call her sons to talk about getting her into assisted living.
I asked if there was anything new that had been happening. She said the only thing that had changed in her life was that she had decided to renovate the house she was living in and that the walls were being torn out. She told me that she smelled mold and that mold had been found behind several walls.
I was like, “Oh, okay, mold. I’ve heard of this before.”
Finally it occurred to me that maybe this was really a mold patient.
We started reading Dr. Shoemaker’s book Mold Warriors together. We found the list of the symptoms. She read them and said, “Oh, I have ice pick pains” and “Oh, I have all the mental symptoms of the brain fog and I’ve been urinating and my stomach’s been hurting.” She was about to see a GI person to get a workup for stomach pains.
She was presenting to me as a psychiatrist with confusion, severe brain fog and an increase in her depression. But she actually had multiple symptoms and had seen many doctors now. Nobody had been able to help her with anything.
We read a little further in Dr. Shoemaker’s book, and I said, “Cholestyramine seems pretty innocuous to use, I’ll try it for you.” So I gave her a prescription for cholestyramine and told her to take it three to four times a day.
She came back three weeks later and I was looking at a different person. It was a very startling experience. She was on time for her appointment, looking alert and put together. She was coherent and neatly dressed. It was like a really different person.
The only thing that had been changed was adding cholestyramine. It was very impressive to me that something that I was calling pre-dementia had been eradicated.
Inflammation and Psychiatry
So I got much more interested in mold and I began to read Dr. Shoemaker’s work to learn about biotoxin illness.
What I found after learning how to do these strange labs is that quite a high percentage of my integrative psychiatric patients actually had some degree of biotoxin illness, based on having haplotypes for mold with dreaded genes or very high elevated cytokines.
That certainly wasn’t anything that I’d ever been taught in medical school or continuing education, or in any of the alternative educational experiences that I had pursued. I became really fascinated about exploring the evidence-based literature for some explanation.
What I found is that neuroinflammation — which is mediated by a variety of mechanisms including cytokines — is very widely documented in the psychiatric literature. It’s just that that knowledge isn’t in most clinical practices.
One thing I’d like to point out that is sort of fascinating to me is that Dr. Shoemaker has often said that it’s about 25% of the population that is susceptible to biotoxins. When you add up all the psychiatric illnesses that people are exposed to, it’s actually about 25% of the population that has been diagnosed or is said to have psychiatric illness.
Is that a coincidence? Perhaps. But it’s a very interesting coincidence to me. Because again, there is a very extensive and robust line of research that neurotransmitter theory alone is really insufficient to explain most psychiatric illness — although it does sell SSRI’s quite well.
Autoimmune Disease, Infectious Illness and Mood Disorders
There is some very recent research that has come out on inflammation and depression. It is from Denmark, which is considered a homogeneous population. They had access to records of 3 million people. (1)
They showed there that if you had a diagnosis of either autoimmune disease — which would include things like Hashimoto’s or rheumatoid arthritis or Sjogren’s — it actually increased risk of being diagnosed with some sort of a mood disorder like depression by 45%. If you’d been hospitalized for some sort of infectious illness, that increased your risk of having mood disorders by 62%. And if you had both of those things happen to you, you doubled your risk of subsequently being diagnosed with a mood illness.
Infections and Toxins
Some of the infections and toxins that we know are associated with depression and anxiety are molds. Neurological Lyme is also well known for creating psychiatric complications. There is good evidence that streptococcus infections not treated properly can lead to obsessive-compulsive disorder, also called PANDAS.
Another source of psychiatric illness are encephalopathies such as Rocky Mountain Spotted Fever that get into the spinal cord. Later or at the same time, people will be diagnosed with psychiatric illnesses including mania.
Toxoplasmosis is associated with cats. There is a large literature that it is associated with an increase in suicides. It’s also increased in schizophrenia.
That’s very fascinating research, because it also has been shown to change the personality of men and women who are infected with it.
The ways that we can see this leading to an inflammation of the brain would be cytokines such as MMP9 and TGF-beta; vasculitis, which is inflammation of the blood vessels; and microglial activation, which are the immune cells of the brain.
Autoimmune disease such as Hashimoto’s can lead to an encephalopathy.
And then something that we’re just going to call excitotoxicity, which is an increase in glutamate in the brain.
Mold and Depression
There is one study out on mold and depression. (2) That was done in Europe. The way they tested for mold was that the researchers just looked at the house, and if they saw mold on the walls or they smelled it strongly, that was called a moldy house. There were no ERMI’s or HERTSMI’s done.
They found surveying people about symptoms of depression that the level of depression in these people living in visibly moldy households was about 34-40% higher than for residents in mold-free dwellings. That was on 6,000 European adults. That’s a pretty good study in a pretty good journal. So that is pretty good evidence that mold does increase the probability of fulfilling the diagnosis for depression.
Sickness Behavior
If you have a number of somatic complaints that a doctor cannot find any physical basis for — or even if they can find a reason for why you have back pain or other problems — and you have any sort of sad mood or not wanting to be out with others, you’re going to be diagnosed as depressed or anxious and given an antidepressant.
But what I want to distinguish here is something called “sickness behavior,” that is very similar to what we diagnose now in DSM-4 as depression. (3)
It’s well-known in the animal literature.
Many of you own a cat. Have you ever had the following experience?
You go to feed your cat and you call her. You don’t see her. You look at her food bowl and realize she hasn’t eaten any food in a few days. You start to get worried and look all over the house for the cat. Finally you find her in some closet you even forgot you had, way in the back. You shine the flashlight and see the eyes, and you think, “Oh, there she is.” You reach down to pet her and she hisses and backs away, further back into the corner. You bring her some food or water and she refuses it. You bring some of her little toys that usually make her happy and there’s no response.
What do you do?
Do you call the cat psychic, which we have a lot of out here on the west coast? Probably not.
You probably do what most people do, which is to call the vet and reach back in there with some gloves to pull her out because she’s probably pretty mad, and put her in a cat cage, and bring her in to find out what is wrong.
There’s always going to be something wrong when a cat is doing that.
What the cat is doing is exhibiting sickness behavior. It’s associated with high cytokines. We measure it in mold illness with MMP9 and TGF-beta and C4a in particular.
But in people, when we see the same behaviors — loss of appetite, reclusiveness, lack of pleasure in usual things, fatigue, irritability — we label that as depression.
What I find many times when talking to patients who come to me for depression is that they initially came to their doctors complaining of not feeling well, hurting, not wanting to do things, not having energy. And because nobody could find a physical basis doing things in a very traditional way, they were pretty much told, “Oh, we don’t know what’s wrong with you, this is all in your head. I think you’d better see a psychiatrist.”
I tend to be one of those psychiatrists that people come to see.
It’s a bit of a joke around here that finally people break down and consult a psychiatrist, and they find the one psychiatrist who says, “No, this isn’t in your head at all. You probably have biotoxin illness.”
Cytokines and Depression
We’re going to talk more specifically now about cytokines and depression. These are references that I can give you to look up, in which they’ve done study of major depression and cytokines. There are at least 24 reports in one of them showing significantly higher concentrations of the inflammatory cytokines. (4, 5)
In these studies, there’s Tumor Necrosis Factor and Interleukin-6, compared with depressed subjects. Dr. Shoemaker has not found those to be particularly useful or easy to measure because of various difficulties. But they are associated with some of the things that he does measure.
So there is some of your first evidence that depression does seem to be a pro-inflammatory state in many people.
Treatment-resistant depression is the technical term for what people have when they come to see me. After two trials of anti-depressants with no response, you’re usually considered to be treatment-resistant. I would prefer to call it “incorrectly diagnosed,” but that’s the label that’s used. And then you’re referred out for more specific treatment, to a psychiatrist, usually.
Here’s more evidence that cytokines are associated with treatment-resistant depression. (6) They actually tend to decrease the expression and function of serotonin. Serotonin is one of the neurotransmitters that is popularly associated with depression but is probably not the cause of depression.
Vaccine Response
There is another study about depression and immune function. (7) They give adults a vaccine. Those who have been diagnosed as depressed do not respond nearly as well to the vaccine, do not mount the antibody response they are looking for nearly as well as those people who do not have a diagnosis of depression or who have had depression and have been treated successfully.
So having depression concurrent with any sort of immune disorder is probably going to lower your chances of getting treated successfully for the immune disorder as well as for the depression.
Hypothalamic-Pituitary Axis
Here’s some more basic science about what we are looking for in the brain when we talk about inflammation. This is a diagram of your brain. It’s looking at your hypothalamus and pituitary.
When you look at Dr. Shoemaker’s model, he’s going to start with damage in the hypothalamic-pituitary axis. It’s that damage that leads to the decrease in hormones that we often see — the decrease in androgens, the decrease in cortisol. Sometimes, as Dr. Shoemaker will say, you’ll see an increase in cortisol, which is your body’s last fling at trying to correct things before you sink into the decreasing cortisol.
This diagram shows the relationship between cortisol and brain inflammation and the cascade of events that happen subsequent to stress.
In this diagram it’s labeled as stress. Stress can be from many different things, such as interpersonal difficulties.
Early adversity is something that is well-studied in psychiatry. Having abusive childhoods is very common, more common than anyone would like to think. This will lead to changes in our ability to secrete cortisol.
This leads to changes in cytokines of something called Nuclear Factor Kappa Beta. It flourishes. That increases inflammation in the body.
The inflammation in the body leads to excitotoxicity. That’s another word for anxiety, really. It decreases neurotransmitters and also causes depression.
There are several agents that can cause this kind of depression besides stress. Biotoxins would be big ones. Others would be heavy metals, food allergens and viruses.
Kynurenine Pathway
Here is a diagram showing the secretions in the brain causing inflammation that is otherwise known as excitotoxicity in the brain. The end result would be increases in depression and anxiety.
This is the kynurenine pathway. It’s a little complicated, but what it’s showing is that in the presence of cytokines, we have tryptophan which is the precursor for serotonin. That is the neurotransmitter associated with depression, that all of the SSRI’s that are antidepressant agents work with.
Tryptophan is decreased or degraded in something called quinolinic acid, which is highly inflammatory. It’s involved in Alzheimer’s, Parkinson’s, Huntington’s, even suicide. It’s very potent and is well-studied as a cause of inflammation leading to neuropsychiatric symptoms.
Here’s a recent study looking at the cerebrospinal fluid obtained through a spinal tap of people who have made suicide attempts and survived. (8) They found that there was a significantly increased amount of quinolinic acid in the cerebrospinal fluid of these patients.
One of the reason this happens is that it antagonizes the glutamatergic pathway. It involves the NMDA receptors, which are highly associated with inflammation. Psychosis actually, and probably suicide.
This study concluded that there is a low-grade inflammation in the brain in suicide victims.
I have patients who will walk into moldy places and their first sign that something is wrong is that they do start thinking about suicide. That’s something that we don’t talk about much but that I do see fairly frequently.
This is not just psychological. There is a state probably of inflammation associated with starting to think suicidal thoughts.
That is something that if you have it, you really need to be talking to someone about it because obviously there are treatments. It’s preventable.
Everyone can find reasons why their life is worth living. Knowing that something in the brain is causing that problem sometimes really helps people to shrug it off and say, “Here come those silly thoughts again. Let me try to figure out what’s going on. Maybe I’m being exposed to mold. Maybe I’m not doing my mold treatments the way that I should be.”
Leaky Brain
Another term for neuroinflammation among alternative integrative doctors is “leaky brain.”
It’s similar to leaky gut in that membranes that are supposed to protect one part of the body don’t work and become increasingly permeable, letting in substances that should have stayed outside.
Cytokines have been shown to increase the permeability of the blood-brain barrier membrane. There’s several ways they do it. Inflammatory cytokines like IL-1, IL-6 and TNF, bacterial toxins, MMP9 and TGF-beta have all been associated with increasing that permeability of the brain.
When we increase the permeability and we increase the stress response of the hypopituitary axis, this is probably going to lead to a breakdown of serotonin in the brain by breaking down tryptophan.
Thyroid Hormones
One other thing that often times happens is that cytokines decrease the conversion of T4 to T3. T3 is the active component of thyroid. You can take a lot of T4 (which is known as Synthroid), but if your body is not converting it to T3, you’re not going to get the benefits of thyroid hormone.
Thyroid hormone is very responsible for mood. It’s a well-known and standard treatment in psychiatry to add T3 to the treatment of people who have what we call treatment-resistant depression. That has often been found to help.
People who have treatment-resistant depression may have neuroinflammation and are not converting their thyroid hormones properly. Adding the T3 their bodies need may be all that they need to correct the depression.
Psychosis
Psychosis is associated with neuroinflammation. That literature is increasing. (9)
I do see people who are psychotic. I’m not going to say that mold causes manic psychosis or depressed psychosis, but I think it very clearly exacerbates that psychosis. Getting people out of exposure and treating the mold does seem to help get people restored to normal brain function.
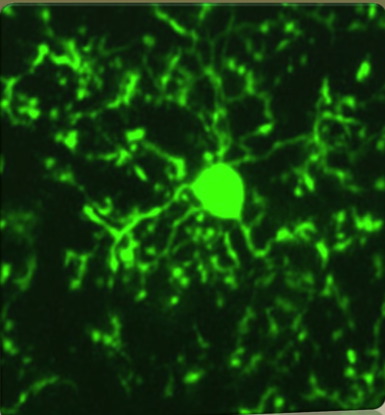
Microglia
This slide shows a picture of microglia in the brain. We have in the brain not only neurons which make our neurotransmitters. We have part of the immune system, which is called microglia. They sort of wrap themselves around the neurons. They are the phagocytes or the macrophages. They are basically what eat viruses and bacteria. They play a key role with regard to inflammation in the brain.
They’ve shown in research that the microglia are activated by head injury and that persistent activation is highly associated with neurodegeneration such as Alzheimer’s. It’s also associated with bipolar disorder.
Bipolar Disorder
Bipolar is also called manic-depression, with alternating moods of depression and mania. There is evidence that bipolar is an inflammatory condition. (10)
In my practice, I have a few bipolar patients. I have one currently who had been treated well for a number of years with traditional medications. He clearly has bipolar, a family history of bipolar. He was exposed to toxic mold, most likely through a flood in the house.
There was a poor remediation. I think we all know about poor remediations here, done quickly through commercial companies. That year, his manias began to get out of control. Meds weren’t working. He was hospitalized and given three potent IV’s of steroids. I think we all know about steroids and mold. That’s not a great idea.
He was finally sent to me by his traditional psychiatrist, saying, “We’re really not helping him here, let’s try something else.” I diagnosed him. He has two dreaded genes.
I’m not going to tell you that adding mold treatment is a miracle, but it is helping and he’s beginning to calm down. It is slow, especially after having had so much exposure to steroids.
He may be one of the first people I know who has been hospitalized and was carried to a psychiatric ward carrying a copy of Surviving Mold, very convinced this is part of his problem.
So that’s one story that I can add to my experience with bipolar mold. There are several other patients that I’ve treated not quite as dramatically. As we begin to treat the bipolar and the mold illness, they are finding clarity of thought and a release from their symptoms that they haven’t had otherwise.
Schizophrenia
There’s some really good evidence, probably some of the best evidence in psychiatry, that schizophrenia is associated with some sort of infectious agent and with inflammatory condition. (11)
In a very large recent study of schizophrenics and antipsychotics, one of the most positive findings they found in the whole study was that almost a quarter of the schizophrenics actually had IGA anti-gliadin antibodies, compared to about 3% of the population. And 5% had high tTG antibodies compared to about 0.8% of the comparison group. Those findings were considered significant enough that I believe that NIH is continuing that study and looking at gluten sensitivity in schizophrenics.
The take home here is that if you know anyone with a diagnosis of schizophrenia, getting them off gluten may really help. Again, not a cure, but it may help.
Again, it’s another psychiatric illness showing an association with inflammation.
Cognitive Impairments
I want to talk about some of the cognitive impairments. Again, that’s associated with brain dysfunction that is also associated with mold. (12, 13)
The most common complaint that I hear from people who are coming to me for depression and anxiety, after their fatigue, is that they say, “My brain just doesn’t work the way it used to.”
There are a number of studies that are validating that observation. There are some studies by psychologists showing clear cognitive impairment associated with mold. There is basic science research showing that mycotoxins excreted by mold are clearly neurotoxic. (14)
Trichothecenes such as are made by Stachybotrys actually kill off the olfactory neurons. Perhaps that’s one of the reasons that we see multiple chemical sensitivity in so many people.
T-2 from Fusarium just kills normal brain cells indiscriminately.
Ochratoxin, associated with Aspergillus, actually depletes the striatal dopamine. That is highly associated with mood disorders and also movement disorders such as Parkinson’s. It also depletes the hippocampus, which is very much where our memory is involved. That is pretty good evidence that ochratoxin is going to be damaging the parts of the brain that are associated with mood and movement disorders.
Executive Functioning
There’s another neurotoxin called fumonisin which also induces neuronal degeneration in the cerebral cortex. That’s your executive function. Some of the studies in mold and many clinical reports show that patients with what we finally call moldy brain have a loss of executive control.
Executive functioning is the part of the brain that looks at all the information coming in and listens to all the different components of the brain.
There’s one part of your brain that’s more emotional, saying, “I hate that person, that person is really saying things that bother me, I need to tell them how stupid they are.” And then there’s the executive part of the brain which computes that and says, “You know, it’s true, that person is not particularly bright, but if we say that, he’s the boss and we’re going to get into fights, and we might lose our job, and is it really worth it?”
It computes all the different possibilities and makes a program to follow that would be the most efficacious way to handle the problem.
In people who lose executive control, you’ll often find them blurting out exactly what they think, which can make them appear fairly irritable and angry to the rest of the world. You’ll also find them asking questions over and over again. Questions are asked and answered, then five minutes later, the same question is asked.
Some of my first mold patients, particularly men, had been referred to me for anger management.
Losing IQ Points
There’s another study that’s come out in the last couple of years that measured cognitive declines in six year olds. This was another study out of Europe, in Poland. (15)
They measured almost 300 kids living in homes with visible mold. This is the researcher going in and seeing mold on the wall and saying it’s a moldy home.
They were following this for allergens and asthma, but they did do psychological testing. They found that after six years, the IQ scores of these Polish children had actually declined 10 points compared to other children followed at the same time who had not been exposed to mold. Kids who had been exposed to mold for three years and then gotten out of those homes showed a decline of about five points.
The reason I bring this up is that this is a significant decline in IQ. The median IQ was 120, which is actually higher than it is in the US at 100.
Losing 10 points would be a lot for anybody.
Neuroplasticity
Now we’re going to talk about neuroplasticity and gaining it back when you’re removed from mold exposures. Don’t panic, but it is something to think about in anybody’s brain.
There is some research in the Alzheimer’s literature linking Alzheimer’s to neuroinflammation. There is a study out recently that analyzed cytokines in Alzheimer’s disease. (16)
Not only do we have the usual cytokines such as IL-6, Tumor Necrosis Factor and IL-1 — which are more commonly measured than some of the things we do in the Shoemaker protocol — you’ll see that TGF-Beta1 is associated with Alzheimer’s disease.
In fact, when they went in the cerebral spinal fluid, they did find higher concentrations of TGF-beta. So that is a more direct association with cytokines associated with mold.
Brain Changes
Now we get to one of the studies that Dr. Shoemaker has done which is what I would call a missing link, showing that brains exposed to mold do show brain damage or brain changes.
This is people with elevated TGF-beta and MMP9. Dr. Shoemaker has shown in the NeuroQuant studies that we have a swelling of the frontal lobes, the hippocampus and the cerebellum and a shrinkage of the caudate. This correlates somewhat with the basic science that I showed you before where mycotoxins do directly damage the brain. (17)
The frontal lobes are where we find that executive function. That’s the part of the brain that says, let’s stop and think about the implications of thinking this or doing this. Hippocampus is highly associated with mood. Cerebellum is associated with movement disorders. The caudate is very dopamine rich and is highly associated with moods and feeling good.
I think that most of you have heard about studies of cocaine or orgasm, that’s usually associated with high concentrations of dopamine. We would call it our feel-good neurotransmitter. Nobody really wants to have a decrease in dopamine. That is also involved in movement disorders such as Parkinson’s.
Diagnosis
All treatment of biotoxin illness is going to start with diagnosis. Diagnosis is difficult since we’re not routinely taught this. In fact, most doctors still believe that mold is really not a big deal, that maybe if you’re exposed to gross amounts of mold, and you inhale it, and you have asthma or pulmonary problem, then we can say that mold has been a problem.
But anything else, like fibromyalgia, chronic fatigue, depression or anxiety is not going to be considered caused by mold, traditionally.
However, it’s my experience that neuroinflammation is highly present in people with psychiatric complaints, especially people not easily helped by traditional easily available treatments.
Some of the clues for when you should be considering the diagnosis of biotoxin illness or neuroinflammation is no family history and age of presentation.
If somebody comes to me complaining of symptoms of bipolar but they don’t have a family history and it started in their fifties, I’m going to be really suspicious that I’m looking at just a genetically idiosyncratically caused bipolar. I’m going to be looking for other causes. And the big things that I’m going to be looking for are neurotoxins, primarily mold. Perhaps Lyme. And other cerebral insults such as an infarction or something like that.
Anxiety disorders and panic disorders do not start in the fifties. Depression starting after menopause, maybe. But I’m happier when I do a diagnosis of depression when the person had depression before and menopause has made it worse, or they have a family history.
Then for diagnosis, you want to be asking, “Have you been exposed to mold? Have you been bitten by a tick? Did you live in a Lyme endemic area?”
Those questions are rarely asked.
Another issue is unusual reactions to medications. I see a lot of patients like that, who are put on something like Zoloft or Celexa and it makes them feel worse. Or they get small amounts of benzodiazapines and feel worse.
That’s actually fairly common.
Often times in medicine when people have unusual reactions to medications, they may be labeled as histrionic, somatacizing, hypochondriacal, whatever. But those kinds of reactions that are labeled as wacky are clues to me that we’re looking at something different and something unusual. And it also makes me think about biotoxin illness.
Case Study
Here is a case of someone who was brought to me about a year ago with severely agitated depression.
She was very reactive during the monsoons. There was some thunder, and she reacted as if a gun had been shot off next to her head and couldn’t stop trembling for about 10 minutes.
If she had had insurance of any sort of financial resources, I would have hospitalized her. She was that severely sick. Unfortunately, that wasn’t available.
I got the history that this severe anxiety and depression had started about 2 1/2 years ago, around the time of menopause. She also at that time had lost her home in California with the financial crisis. And she also had found out that her husband had a terminal illness related to the lungs.
She had never been depressed or anxious before, in fact had been quite the opposite. But there was a family history of anxiety and depression. She had been treated in California by several psychiatrists for hormones and for the psychiatric illness, without any improvement.
She had had severe GI pain. When they investigated, they blamed it on diverticulitis. Surgeons wanted to remove a foot of her colon. The family didn’t have the money and the patient didn’t want that done, so they refused the surgery. That was interesting to me, because usually when surgeons want to remove a foot of your colon, you don’t recover without any sequelae and then function normally for the next year.
They moved to Arizona to be with family and the husband became the full-time caretaker of the wife. He had to be with her day and night, watching her. She did feel suicidal. She couldn’t function. She’d be up and pacing all day, severely anxious and really not capable of doing anything else.
I was seen as the last resort, which unfortunately is what happens in integrated psychiatry since meds haven’t helped.
I ended up changing the psychiatric meds, which led to a partial improvement in the first month or so. The family was very happy. But unfortunately, that improvement stalled and I spent the next six months just switching meds and adding supplements without much more improvement. We didn’t have to hospitalize her, but there was very little quality of life for her or for the husband.
Then again in summer, she worsened considerably. The depression and anxiety became much more unmanageable.
She had a colonoscopy that showed no problems — no cancer, no necrosis. That was again a little puzzling and interesting to me.
Out of desperation, I started to ask about mold. If people are very psychiatrically ill and you start asking about mold, they have a hard time believing it. Sometimes I get a little cautious about bringing it up, because it’s so out there to so many people.
But after a year of treatment, I started asking about mold. That’s because mold illness in Arizona is actually worse in the summer due to our monsoons and swamp coolers and leaking roofs and stuff like that.
The husband remembered that at about the same time that his wife became very ill, he had found extensive black mold in the garage due to a leak in the kitchen sink above. The house was in disrepair because of financial crisis. He had done the remediation himself without any precautions before doing a short sale. He felt that the mold had been there for a few years because the house was a fixer-upper that they were fixing up to be their dream house.
So he got interested because he has an alpha antitrypsin deficiency that can lead to lung problems. He knew that he shouldn’t be exposed to mold. He became very interested and read Surviving Mold. He had his wife do the visual contrast tests and she failed.
I started cholestyramine. They didn’t have money really for insurance, but I got a haplotype that showed that she did have a mold gene and a low MSH gene.
I saw her a month later. This was the first time she had ever been able to talk to me without tears or agitation or having to be forced to talk. She was actually talking freely, talking about her experience. She told me that she was very tired from cholestyramine, but that she had actually had waves of feeling herself again.
Interestingly enough, the husband at the VA had a CT scan which showed in his lungs sarcoidosis and possible fungal balls. So he was fairly grateful to have learned about mold too.
I’m sharing this case just to show that I did not initially pick up symptoms of mold because the psychiatric presentation was so dramatic that I went immediately to psychiatric meds without talking about mold. Obviously if I didn’t ask about mold, there are very few psychiatrists who would have asked her.
It does now look like this was contributing. The CSM was the first treatment where she got periods of time when she was feeling like herself.
I assumed this was due to family stressors and the onset of menopause and traumatic life events. I was wrong.
I will point out that her response to SSRI’s was typical of the mold patient in that they made her worse, agitated her more, didn’t work really at all.
Treatment
I’d like to make it obvious. I am not against using allopathic meds. If somebody is feeling very depressed or anxious, I’m going to do whatever I can do to alleviate suffering.
I will not tell people to get off their meds when I diagnose mold illness. I suggest that they work with me to treat it and gradually go off meds so that we don’t have any exacerbations of symptoms of depression.
Mold treatments that I use that are pretty easily available are, of course, the whole Shoemaker protocol.
Fish Oil
Another supplement that Dr. Shoemaker recommends highly for inflammation is fish oil. There’s actually a large psychiatric literature that fish oil helps, to the extent that even the American Psychiatric Association endorses the use of fish oil in psychiatric illness. It’s safe and effective. Fish oil is not something that you would think of, but in some studies a three-month course of fish oil seemed to be actually as effective as drugs in cutting the rate of psychotic illness and schizophrenia, by almost 25%. (18)
You have to understand that in your brain, you have neurons that are your electrical system. Neurons are surrounded by a myelin sheath, which is your insulation for nerve wires. That myelin sheath is a fatty substance that is highly improved by adding the EPA, DHA and other cholines. It’s called the phospholipid bilayer cushion. That’s what we believe fish oil may be doing.
Other things that fish oil has been shown to do is that it allows serotonin and dopamine, your neurotransmitters, to bind to receptors. It down regulates cortisol, which is very high in stress and is the response from the adrenals before adrenal fatigue sets in. There’s no evidence that it decreases cortisol, so don’t be afraid to use it if you have low cortisol.
It down regulates inflammatory cytokines. It actually helps increase thyroid hormone transfer to the brain.
There’s a pretty good literature on Omega-3’s in bipolar illness. I often find it almost diagnostic when I give people a liquid fish oil, pharmaceutical grade, and people with bipolar illness will guzzle it when they’re not feeling well and feel that they can almost regulate their illness by using fish oil.
Diet
Very, very important is diet. I am very big on the anti-inflammatory diet, meaning anti-inflammatory for the brain.
There’s a study that looks at whether Alzheimer’s Disease can be a form of Type-3 Diabetes. Alzheimer’s may be very strongly linked to inflammation from sugars. (19)
The type of diet that I recommend is one that is low in sugars. Low in processed sugars and also low in carbs, because carbs are broken down to simple sugars. It may be Dr. Shoemaker’s amylose-free, which has you off most grains and amylose.
You can call it the ketogenic diet. The ketogenic diet is one that switches you over from burning carbs to burning fat.
That diet has been used for almost 100 years to treat epilepsy in children. It really does work. We wouldn’t be doing it for 100 years if it didn’t. Johns Hopkins is actually at the forefront of doing that for the last 100 years.
The ketogenic diet is probably the one that is best for the brain. It’s also known as the Paleo diet. The goal is to start eliminating sugars and simple carbs from your diet.
If you want to read a recent book, it would be Dr. Perlmutter’s book “Grain Brain” and all of his work on the topic of carbohydrate excess on brain function. You also can look on my blog in the article about “Ketogenic Resources” and then just start to follow all the links about the ketogenic diet. (20)
I’m also a very big believer in eliminating food sensitivities such as gluten and dairy. Again, those contribute to inflammation including probably neuroinflammation.
Gluten sensitivity in celiac has been known for a long time to cause something called gluten ataxia, which is balance. That is just one study that shows that gluten sensitivity can affect the brain.
I tell most people to get off gluten and dairy initially. Many people do feel better. For others, the benefits may not be shown for many months. Or they may find that when they start to do gluten or dairy again, things get worse for them. This is a fairly simple trial that everyone suffering from some kind of chronic inflammatory illness should be trying.
Again, I’m mentioning the schizophrenia and the anti-gliadin antibodies which is pretty impressive actually.
Bipolar illness is very linked to epileptic illness. They use the same drugs to treat them and they are effective in bipolar illness.
The ketogenic diet is effective in epilepsy in children. There are some small studies showing that based on that reasoning, the ketogenic diet might help bipolar brains.
There are some small studies showing that to be true. It’s something that I do recommend for people with bipolar illness, especially when people are having a hard time trying to control it.
So diet to me is extremely important. When you have something like Chronic Inflammatory Response Syndrome affecting so many areas of your life, there is no magic bullet here. The treatment works but it can be slow. Doing the diet changes can significantly help decrease inflammation throughout the body.
Supplements
A natural substance that you can take that are effective for the brain would be magnesium. Many Americans are very deficient in magnesium.
A number of cases have been documented showing rapid recovery from depression when magnesium was supplemented. (21)
Magnesium deficiency is linked to an increased risk for stroke. It’s linked to glutamate excitability. Magnesium does help decrease glutamate in the brain. Glutamate is highly associated with anxiety.
I recommend magnesium for anyone with problems with insomnia or anxiety. For hypertension, it’s excellent. It’s something that should be tried in hypertension.
We also use it a lot when people are taking cholestyramine, which is highly constipating. We have patients mix powdered magnesium citrate directly with the cholestyramine. We find that solves most people’s problems with constipation.
Another effective substance is tumeric. There’s one study showing that 1000 mg of tumeric taken over six weeks was as effective as Prozac in depression. (22) To me, since tumeric is highly anti-inflammatory, that’s another study suggesting that for many people, depression is a condition of inflammation.
Probiotics are very very useful. MSH, which is low in many people, is going to mediate the tight junctions between cells and contribute to leaky gut. There’s a strong connection between pathogenic gut, bacteria and anxiety. (23, 24) I have certainly seen a number of times that adding probiotics can help anxiety and depression.
Vitamin D is highly linked in many studies with depression and anxiety. (25) It is, of course, linked with the immune system. It can improve the immune system and is cancer protective. Levels are easily measured. I think that Dr. Shoemaker showed low Vitamin D levels in patients and that those levels improves with VIP without supplementation.
When I measure low Vitamin D levels, I will always encourage people to get on Vitamin D. 5000 is my usual dosage. For people with very low levels, we may go as high as 10,000. With some people, we will just use 1,000. And yes, this is even in sunny Tucson. Studies have shown that 70% of people here in Tucson have Vitamin D deficiencies. There’s more to Vitamin D than just the sun.
There are a couple of studies linking Vitamin D and depression.
Selfish vs. Eudaimonic Happiness
There are a number of studies linking happiness — psychological states and behaviors — at the genetic level with inflammation. (26) This research is known of as the field of epigenetics. It’s showing that it’s possible to alter the expression of inflammation at the genetic level. These are not just psychological changes — it actually showed decreased expression of proteins responsible for inflammation.
Psychological researchers have differentiated between different types of happiness. There’s a happiness that is known as more selfish happiness. You might think of that as coming home, watching a TV program you like, having some alcohol, eating some food, maybe doing something else associated with pleasure. Those things make you happy, but do not necessarily contribute to the meaning of life or help other people. That’s considered more selfish happiness.
Buying cars or having nice clothing perhaps would be considered more hedonic happiness.
Eudaimonic happiness is associated with having a sense of meaning and purpose in life. That can be different in everybody. That could be taking care of your family, taking care of your children. That would certainly be noble purpose. It could be social happiness — being involved in groups with other people, communicating with other people, feeling that your experience helps other people. That would be associated with more eudaimonic happiness.
You don’t have to be a Mother Teresa, which is the first thing that most people will think about with eudaimonic happiness. But again, it’s having a sense of meaning and purpose to your life that differs across people but is a feeling that people have. That has been shown to decrease the expression of the pro-inflammatory genes and actually increase the expression of genes responsible for killing viruses and bacteria directly.
Nobody knows exactly why this happens, but it probably is linked somehow to the survival of the species and survival of us as a group, as opposed to individual survival.
I will have to say in my practice that people who have some meaning in their life — who are linked to family or linked to church or linked to work that they feel is meaningful — do sometimes do better than people who are very isolated and who have lost feeling that what they do matters very much in the world.
Other non-pharmacological things that may help with things like marrow plasticity (which means getting your brain to grow new brain cells) or parasympathetic output (which is linked to relaxation) would be mindfulness meditation. There’s a lot of research now on the benefits of mindfulness meditation or even mindfulness psychotherapy. (27)
Recovery
In my practice, treating biotoxin illness for several years, I’d say that a large percentage of the patients that I see who are complaining initially about depression and anxiety and insomnia — when we start the appropriate treatments with the Shoemaker protocol, their problems just gradually resolve over 2-4 months. It just becomes a non-issue. In fact, sometimes we have to go back to the initial notes and remind people that they first came to me because they were complaining about depression or anxiety.
I would say that about 30% are going to need more intensive supplemental or allopathic intervention. Again, I am not opposed at all to using benzodiazapines or SSRI’s or stronger meds if they are needed.
I think therapy or support can be very helpful. I often refer people to a psychologist who is very familiar with mold illness.
Patients find it very helpful that they can talk to someone who doesn’t think they’re crazy when they start talking about their mold treatment or when they link re-exposure to psychiatric symptoms. I hope there are more and more psychologists who will be available to do that. Or coaches who have experience. It is extremely helpful for people going through this.
There are about 10% of people that I see who have what I would call intense psychiatric processes going along, such as severe agitation, depression or psychosis. They may require antipsychotics or even electroconvulsive therapy. Although it sounds severe, when there is severe suicidal ideation or when people aren’t eating — when there’s a threat to life — what’s needed needs to be done.
Thank you for letting me share what is for me exciting and interesting information.
*
References:
(1) Benros ME, Waltoft BL, Nordentoft M, Ostergaard SD, Eaton WW, Krogh J, Mortensen PB. Autoimmune diseases and severe infections as risk factors for mood disorders: a nationwide study. JAMA Psychiatry, 2013 Aug; 70(8): 812-20.
(2) Shenassa ED, Daskalakis C, Liebhaber A, Braubach M, Brown M. Dampness and mold in the home and depression: an examination of mold-related illness and perceived control of oneʼs home as possible depression pathways. Am J Public Health. 2007 Oct; 97(10): 1893-9.
(3) Arnett SV, Clark IA. Inflammatory fatigue and sickness behaviour – lessons for the diagnosis and management of chronic fatigue syndrome. J Affect Disord. 2012 Dec 10; 141(2-3):130-42.
(4) Gardner A, Boles RG. Beyond the serotonin hypothesis: mitochondria, inflammation and neurodegeneration in major depression and affective spectrum disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2011 Apr 29; 35(3): 730-43.
(5) Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctot KL. A metanalysis of cytokines in major depression. Biol Psychiatry. 2010 Mar 1; 67(5): 446-57.
(6) Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009; 65:732-41
(7) Irwin MR, Levin MJ, Laudenslager ML, Olmstead R, Lucko A, Lang N, Carrillo C, Stanley HA, Caulfield MJ, Weinberg A, Chan IS, Clair J, Smith JG, Marchese RD, Williams HM, Beck DJ, McCook PT, Zhang JH, Johnson G, Oxman. Varicella zoster virus-specific immune responses to a herpes zoster vaccine in elderly recipients with major depression and the impact of antidepressant medications. Cln Infect Dis. 2013 Apr; 56(8):1085-93.
(8) Erhardt S, Lim CK, Linderholm KR, Janelidize S, Lindqvist D, Samuelsson M, Lundberg K, Postolache TT, Traskman-Bendz L, Guillemin GJ, Brundin L. Connecting inflammation with glutamate agonism in suicidality. Neuropsychopharmacology. 2013 Apr; 38(5): 743-52.
(9) Tatiana Falcone T, Carlton E, Franco K, Janigro D. Inflammation, psychosis and the brain. Psychiatric Times 2009; 26.
(10) Stertz L, Magalhaes PV, Kapczinski F. Is bipolar disorder an inflammatory condition? The relevance of microglial activation. Curr Opin Psychiatry. 2013; 26:19-26.
(11) Cascella NG, Santora D, Gregory P, Kelly DL, Fasano A, Eaton WW. Increased prevalence of transglutaminase 6 antibodies in sera from schizophrenia patients. Schizophr Bull. 2013 Jul; 39(4):867-71.
(12) Crago BR, Gray MR, Nelson LA, Davis M, Arnold L, Thrasher JD. Psychological, neuropsychological and electrocortical effects of mixed mold exposure. Arch Environ Health. 2003 Aug; 58(8): 452-63.
(13) Gordon WA, Cantor JB, Johanning E, Charatz HJ, Ashman TA, Breeze JL, Haddad L, Abramowitz S. Cognitive impairment associated with toxigenic fungal exposure: a replication and extension of previous findings. Appl Neuropsychol. 2004;11(2): 65-74.
(14) Doi K, Uetsuka K. Mechanisms of Mycotoxin-Induced Neurotoxicity Through Oxidative Stress-Associated Pathways. Int J Mol Sci. 2011; 12(8):5213-37.
(15) Jedrychowski W, Maugeri U, Perera F, Stigter L, Jankowski J, Butscher M, Mroz E, Flak E, Skarupa A, Sowa A. Cognitive function of 6-year-old children exposed to mold-contaminated homes in early postnatal period. Prospective birth cohort study in Poland. Physiol Behav. 2011 Oct 24: 104(5):989-95.
(16) Swardfager W, Lanctot K, Rothenburg L, Wong A, Cappell J, Hermann N. A metaanalysis of cytokines in Alzheimerʼs disease. Biol Psychiatry. 2010; 68:93041.
(17) http://www.survivingmold.com/diagnosis/neuroquant
(18) Amminger GP, Schafer MR, Papageorgiou K, Kiler CM, Cotton SM, Harrigan SM, Mackinnon A, McGorry PD, Berger GE. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010 Feb; 67(2):146-54.
(19) Accardi G, Caruso C, Colonna-Romano G, Camarda C, Monastero R, Candore G. Can Alzheimer disease be a form of type 3 diabetes? Rejuvenation Res. 2012 Apr; 15(2):217-21.
(20) http://mypassion4health.blogspot.com/2013/09/ketogenic-diet-resources.html
(21) Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Med Hypotheses. 2006; 67(2):362-70.
(22) Braidy N, Grant R, Adams S, Guillermin GJ. Neuroprotective effects of naturally occurring polyphenols on quinolinic acid-induced excitotoxicity in human neurons. FEBS J. 2010 Jan; 277(2):368-82.
(23) Messaoudi M et al. Beneficial psychological effects of a probiotic formulation (lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in healthy human volunteers. Gut Microbes. 2011; 2, 256-261.
(24) Benton D et al. Impact of consuming a milk drink containing a probiotic on mood and cognition. Eur J. Clin Nutr. 2007; 61, 355-361.
(25) Jorde R, Sneve M, Figenschau Y, Svartberg J, Waterloo K. Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: a randomized double blind trial. J Intern Med. 2008 Dec; 264(6):599-609.
(26) Fredrickson BL, Grewen KM, Coffrey KA, Algoe SB, Firestine AM, Arevalo JM, Ma J, Cole SW. A functional genomic perspective on human well-being. Proc Nat Acad Sci USA. 2013 Aug 13;110(33):13684-9.
(27) Pace TW, Negi LT, Adame DD et al. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology. 2009; 34: 87-98.
Like this blog?
Sign up for more information about the role of toxic mold in human health from Paradigm Change here.
*
A PDF version of this article is at this link.
The audio recording of the talk is at this link.
*
To go to the Paradigm Change website, please click here.
*
Any and all comments from actual humans are welcome on this blog. If you submit a comment and it doesn’t go through, please assume that it is due to inappropriate spam filtering and let us know via email at paradigmchange at yahoo.com.
Thanks much for reading this blog.
Rate this article: